A nation under pressure

These datasets, coupled with our unrivalled expertise in blood pressure measurement and monitoring, provide unique insights into public perceptions of blood pressure and enable us to identify gaps in awareness. This report aims to equip individuals and healthcare professionals alike with the knowledge needed to take control of blood pressure and advance Hilo’s mission to protect the nation’s heart health for the future.
Only 47%
of the UK public have heard of ‘hypertension’ and understand what it means, and the rest, over half, are unsure.
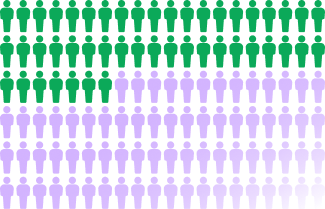

Only 25%
of UK adults have had a diagnosis, but government data suggest that up to a third of adults are known to be affected – a significant diagnosis gap.


Only 25%
of UK adults have had a diagnosis, but government data suggest that up to a third of adults are known to be affected – a significant diagnosis gap.
39%
of young adults aged 16–24 believe there are obvious symptomsof hypertension
Use of a continuous monitoring device is associated with tangible reduction of blood pressure.
Data collected shows that users can halt the dangerous increase in systolic blood pressure usually seen in the over 50s.
Hypertension
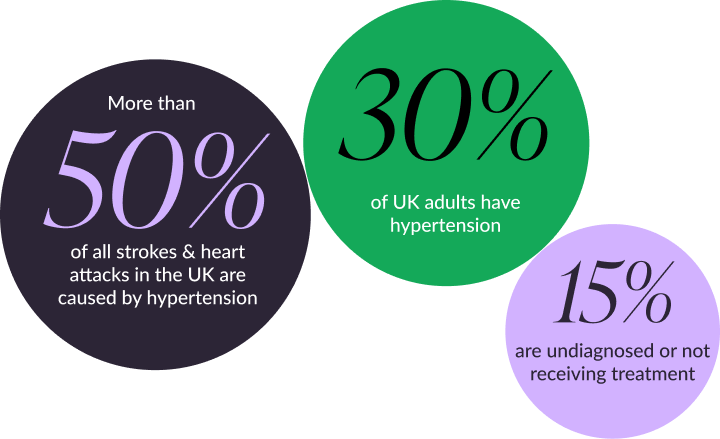
A silent health emergency
- An estimated 30% of UK adults have hypertension,3 but 15% (around 4.2 million people) are either undiagnosed or not receiving treatment.4
- Incidence rises with age: more than half of adults aged 65 and over are affected, compared with just 9% of those aged 16–44.3
- Ethnicity also plays a role, with people from African, Caribbean or South Asian backgrounds at higher risk of developing high blood pressure than the rest of the population.5
With this in mind, Hilo set out to evaluate public attitudes and perceptions towards hypertension using two approaches: proprietary polling through an online UK survey (n = 2,000) and analysis of data from long-term UK users of the Hilo app (n = 8,950). We wanted to understand:
- What people really know about hypertension;
- How seriously it’s taken as a public health condition;
- Public perceptions of symptoms;
- Whether high blood pressure is a worry;
- Whether wearing a Hilo Band influences blood pressure measurements.
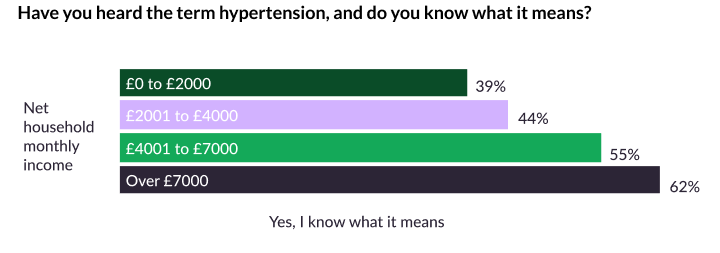
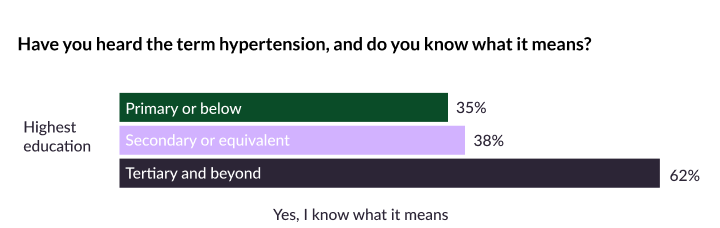
Our research revealed significant gaps in public knowledge and understanding of hypertension – particularly when compared across monthly income and education levels. Worryingly, the findings suggest that many people only take action once hypertension is already established. Yet, for the first time, our data shows that engagement with medical-grade wearable technology brings real benefits: blood pressure increases that are considered normal in later life can be halted or even reversed, challenging the long-held belief that rising blood pressure is an inevitable part of ageing.
The findings from our research were grouped into three main themes: awareness, behaviours, and the impact of long-term monitoring. However, a fourth theme emerged consistently throughout the analysis: awareness and behaviours around blood pressure are closely related to monthly income and level of education. Our data revealed that people from lower-income households, or with lower levels of completed education, are less likely to understand the dangers of high blood pressure and are therefore at greater risk of serious illness from this condition.
Awareness
Age, income and education are key factors
Although hypertension causes more than half of all strokes and heart attacks in the UK, and affects one in three people, only 47% of the public had heard the term ‘hypertension’ and understood what it means.6 Despite this, just over half of respondents recognised it as a serious medical condition, and most could identify its major health risks, such as stroke and heart attack. However, far fewer were aware of its link with other serious illnesses, including kidney disease and vascular dementia.7
These statistics are concerning in themselves, but when monthly income and level of completed education were taken into account, the disparities were striking:
- Those households with lower net monthly income, or those where education was completed only up to secondary level, were significantly less likely to understand what hypertension is or the impact that it has on health.6
UK government guidance states that a diagnosis of hypertension applies when blood pressure is above 140/90 in a medical setting.8 Most people surveyed (55%) stated that they knew what a high blood pressure reading was, with younger adults more likely to make this claim.9 However, when asked to give a value, the median response across all participants was 162/92 mmHg – and even higher for those under 34 – revealing a clear disconnect between medical guidelines and public perception.
And while 52% of respondents correctly recognised that high blood pressure can only be detected through measurement, nearly a quarter believed it had obvious symptoms – a figure that rose to 39% among young adults aged 16–24.10
Did you know the lesser known effects of hypertension?
- Vision loss and blindness
- Chronic kidney disease and kidney failure
- Vascular dementia and cognitive impairment
- Aortic aneurysm and dissection
- Sexual dysfunction and erectile dysfunction
- Pregnancy complications (preeclampsia, eclampsia)
- Hypertensive crisis with severe headache and nosebleeds

Behaviour
It’s estimated that around one third of adults in the UK have hypertension,3 with incidence increasing with age. About 50% of those living with the condition are thought to be unaware of it and therefore aren’t receiving treatment. This pattern was reflected in our findings: just under a quarter of respondents recalled having a diagnosis, while the majority (over 70%) said they have never received one – indicating that up to 10% of participants may have high blood pressure without knowing it.11
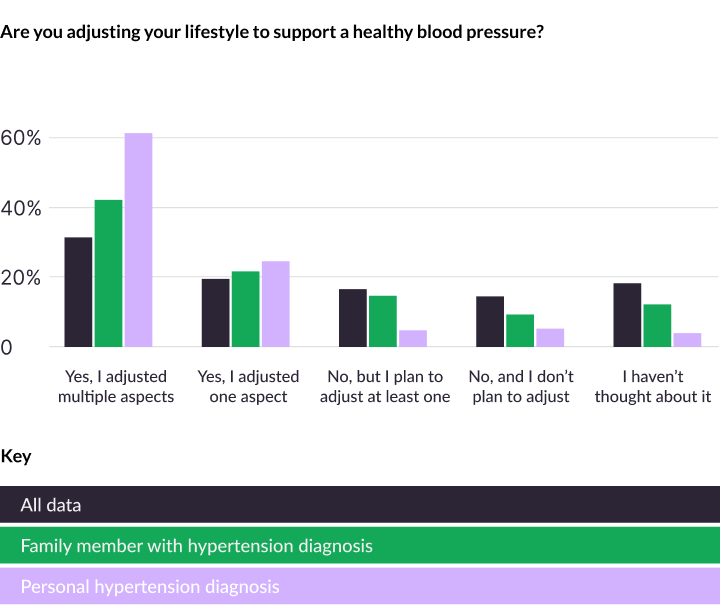
Education and income play an important role in shaping understanding and lifestyle choices. Those from lower-income backgrounds or with a lower level of education were far less likely to have considered the link between lifestyle and blood pressure. The greatest influence on behaviour12 was a hypertension diagnosis – either their own or that of a close family member13 – although this often came with increased worry14.
Diagnosis prompts most people to make lifestyle changes that support heart health, but without that nudge, many might never consider doing so.
Impact
Complacency toward blood pressure monitoring was clear from the frequency of measurement. More than 70% of respondents hadn’t checked their blood pressure within the previous month, and almost one in five had either gone more than two years without doing so, or could not recall when they last measured it.15 Regularity of measurement was related to age, income and education: younger adults, those on lower incomes, and those with lower levels of completed education were less likely to have measured their blood pressure in the past month. However, in line with lifestyle behaviours, diagnosis was a key motivator: regardless of socioeconomic group, people with hypertension, or with a family member who had been diagnosed, were likely to measure blood pressure more regularly.
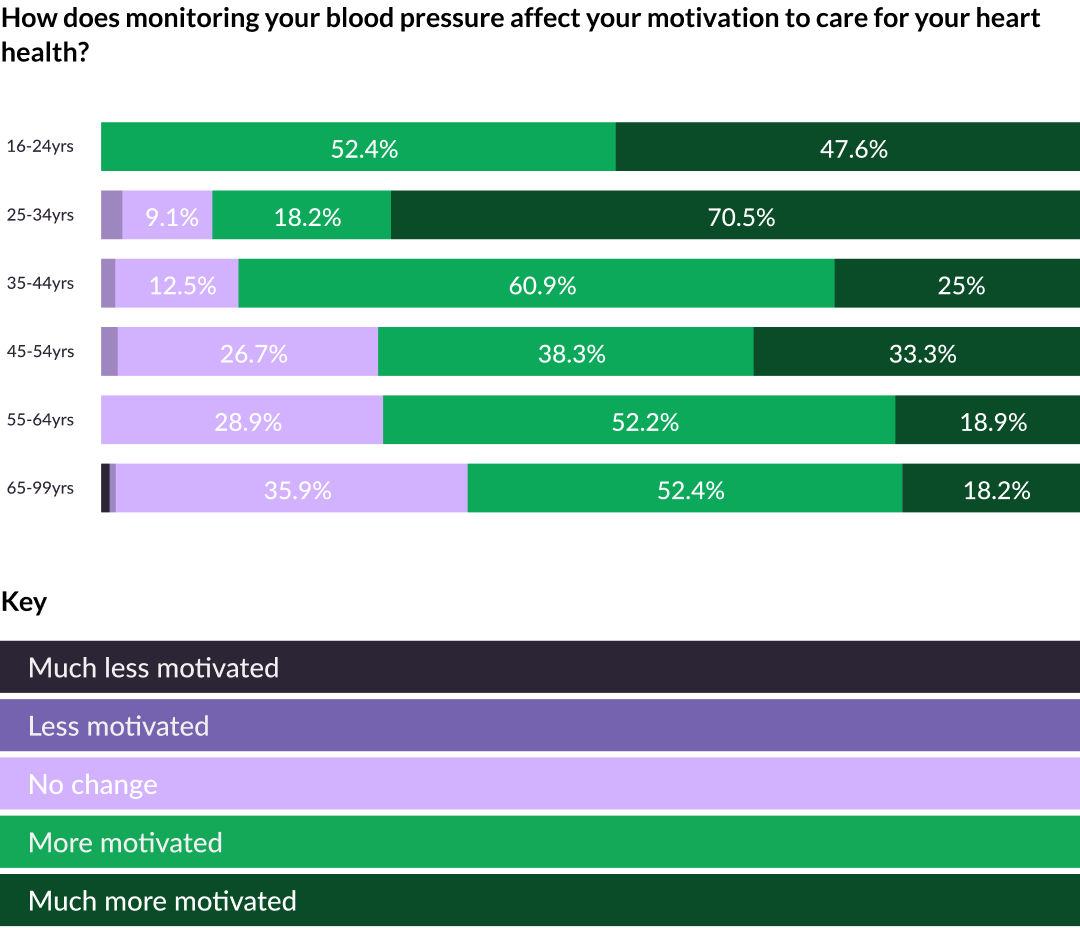
This finding – that blood pressure monitoring can motivate people to look after their heart health – is also reflected in our proprietary user data.
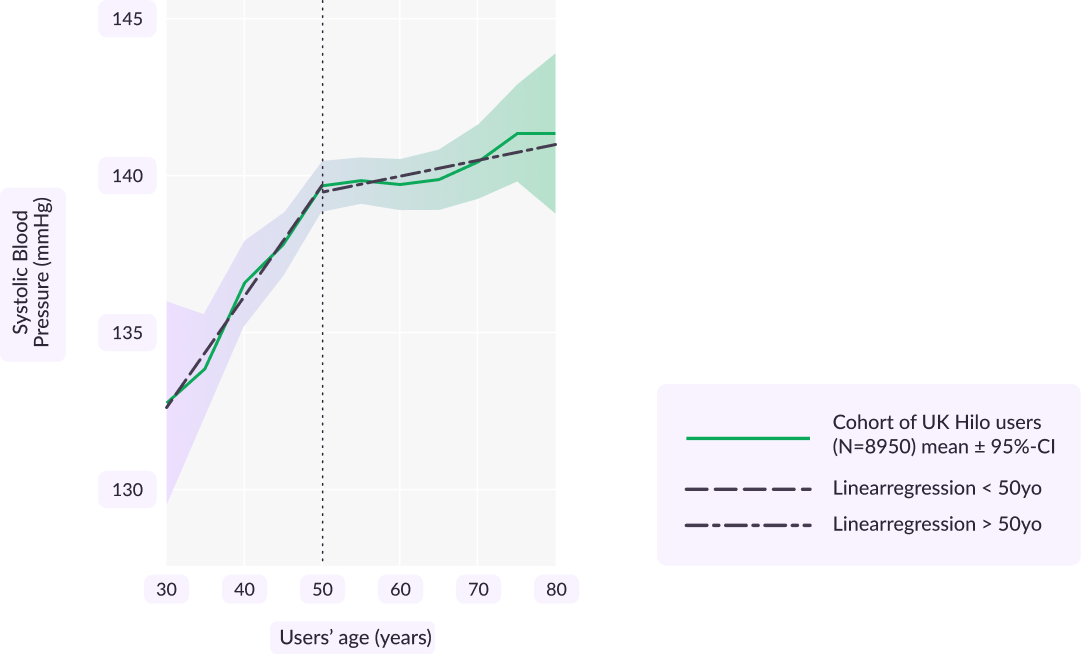
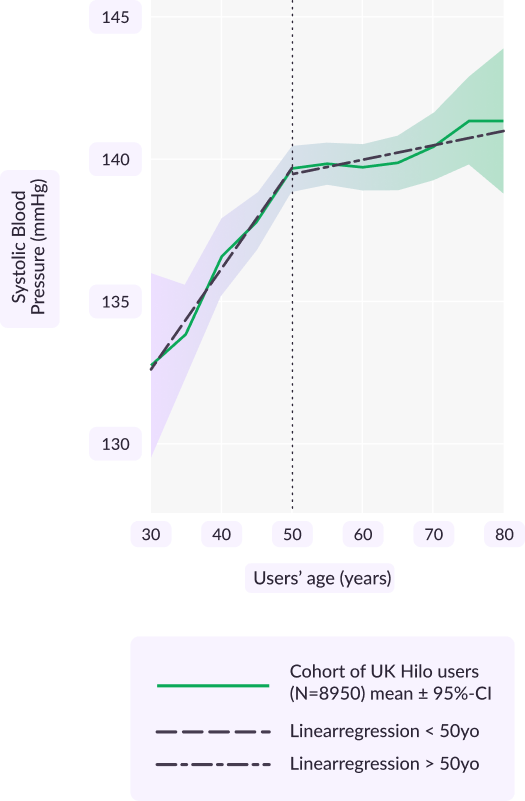
Continuous monitoring helped users aged 50 and above to stabilise their systolic blood pressure levels, defying the increase typically observed in older population.
In addition to these physiological trends, We also observed that hypertensive and older individuals remained engaged with the wearable monitor for longer periods compared to normotensive and younger individuals – a sign of more proactive blood pressure monitoring and greater awareness of cardiovascular risk.
Key takeaways

While most of the public were able to identify the major health risks associated with hypertension – stroke and heart attack – only about half understood the term ‘hypertension’ or recognised it as a risk factor for other serious disease. This lack of understanding was particularly evident among households with lower income or lower levels of education.
A personal hypertension diagnosis – or that of a close family member – had the biggest impact on awareness and understanding. Without this nudge, people from lower socioeconomic backgrounds were far less likely to have recently measured their blood pressure or considered its link with lifestyle, creating a potentially dangerous diagnosis gap.
Around half of respondents owned a blood pressure monitor, but ownership didn’t always translate into use. Younger adults – even in households with a monitor – were less likely to have measured their blood pressure recently, or to have considered taking readings, compared with older adults. They were also the most likely to believe that hypertension has noticeable symptoms. Interestingly, however, younger adults were the most likely to agree that monitoring blood pressure motivated them to care for their heart health – yet they remained the least likely to do it regularly.

Raising awareness of blood pressure increases motivation – and with greater motivation comes real change. At Hilo, we believe that continuous blood pressure monitoring can make a meaningful difference to people’s lives, protecting their hearts and significantly reducing risk of serious long-term illness.
Using a medical-grade device to monitor blood pressure continuously can drive meaningful change and deliver tangible improvements, particularly in systolic blood pressure

For deeper insights, additional data or expert interviews, contact press@aktiia.com. If this report prompts you to consider your own blood pressure, regular monitoring is a powerful first step. To learn how continuous monitoring works and how the Hilo Band can support evidence-based action, visit hilo.com.
Message from Stefan Petzinger


There is a gap between risk and action that is a real problem. And the scale of it surprised us. This isn’t a niche health issue; this affects millions.
Publishing this report is our way of putting the issue on the table. Yes, our mission is to develop tech that helps people control their blood pressure – but the findings point to a broader responsibility. This needs more attention from media, policymakers, clinicians and, frankly, from all of us. Ignoring it just guarantees more avoidable sad events and more avoidable tragic loss.
If this report does one thing, it should be to raise the urgency level. High blood pressure isn’t complex. It’s just not talked about enough. That needs to change.”
Download the 2025 Hilo blood pressure report.
Download PDF



The Hilo Band and what it does
Authors
Dr Tiago Almeida, PhD
Dr Philippa Cranwell, PhD
Dr David Perruchoud, PhD
Dr Josep Solà, PhD
Methodology
To collect and analyse the data, we used several sources:
- UK poll – Nationally representative survey (Appinio, October 2025; n = 2,000).
- Internal data – Anonymised data from long-term UK Hilo users (n = 8,950).
Anonymised data from an external survey:
The external survey was conducted by Appinio through their online platform over four days in October 2025 on behalf of Aktiia SA. Use of data entered by users was included in the Terms & Conditions and Privacy Policy during account setup. UK users were invited to take part in the survey through a notification, and when the threshold of 2,000 responses was met, the poll closed. Participants were aged 16 or over and the survey population was deemed representative of the national UK population. Data were then pooled and analysed.
Proprietary, anonymised data from existing users of the Hilo Band:
British users (n = 8,950) provided informed consent for the retrospective analysis of their anonymised data by voluntarily accepting Hilo’s Terms & Conditions and Privacy Policy during account setup. These documents define the scope, purpose, and lawful basis for the use of such data in retrospective and anonymised research and analytical activities. For inclusion in the study, subjects must have used the Hilo Band for at least six months between 2022 and 2025. Data interrogated included BP values, demographic data (age, gender, BMI) and engagement – i.e., how often they accessed the Hilo app and were exposed to their own BP values. Several analyses were conducted, comparing BP values and engagement within different demographic groups.
References
- Blood Pressure Facts and Figures. Blood Pressure UK. https://www.bloodpressureuk.org/news/media-centre/blood-pressure-facts-and-figures/ (Accessed November 2025)
- Hypertension. World Health Organization, 25 September 2025. https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed November 2025)
- Health Survey for England, 2021 part 2, NHS England, 16 May 2023, https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2021-part-2/adult-health-hypertension (Accessed November 2025)
- A. Leadsom, Get your blood pressure checked, Department of Health and Social Care, UK Government, 11 March 2024. https://www.gov.uk/government/news/get-your-blood-pressure-checked (Accessed November 2025)
- Your ethnic background and your blood pressure. Blood Pressure UK. https://www.bloodpressureuk.org/your-blood-pressure/how-to-lower-your-blood-pressure/healthy-eating/your-ethnic-background-and-your-blood-pressure/ (Accessed November 2025)
- Have you heard of the term hypertension and do you know what it means? Yes, I know what it means, (46.6%); Yes, I’ve heard of it but I’m not sure what it means, (46.4%); I’ve not heard of it (7.1%). Filtered by age/income (n = 2000)
- Which of the following health risks associated with high blood pressure are you aware of? Stroke; hair loss; kidney disease/failure; diabetes; vision loss; increased risk of skin cancer; heart attack; tooth decay/gum disease; vascular dementia/cognitive decline; arthritis/joint pain; none of the above; other. Filtered by age (n = 2000)
- High Blood Pressure. National Health Service (NHS), UK. https://www.nhs.uk/conditions/high-blood-pressure/ (Accessed November 2025)
- Do you know what values are considered as high blood pressure? Yes (55%); no (45%). Filtered by age (n = 2000)
- How straightforward is it to detect high blood pressure without heaving it measured? Straightforward – it has obvious symptoms in most cases; difficult – it often has no symptoms in most cases; not sure. Filtered by age (n = 2000)
- Regardless of your current blood pressure, have you ever been diagnosed with high blood pressure by a healthcare professional? Yes, I have been diagnosed (23.6%); No, I was never diagnosed (71.3%); I don’t know (4.5%); Prefer not to say (0.7%). Filtered by age (n = 2000)
- Are you adjusting your lifestyle to support a healthy blood pressure (e.g. sports, diet, stress)? Multiple answers filtered by hypertension diagnosis (n = 2000).
- Do you have any family members with high blood pressure? Yes (49.1%); No (38.9%); I don’t know (12.1%) (n = 2000)
- To what extent does your blood pressure concern / worry you? Not at all concerned; Slightly concerned; Moderately concerned; Very concerned; Extremely concerned; Not sure. Filtered by family or personal hypertension diagnosis (n = 2000)
- When did you last have your blood pressure measured? Less than 1 month ago; 1–6 months ago; 6 months–2 years ago; more than 2 years ago; never; I don’t know; prefer not to say. Split by age or diagnosis (n = 2000).
- Where did you have your blood pressure measured last? At home (26.5%); doctor (59%); pharmacy (11%); prefer not to say (0.5%); other (3%). (n = 1821)
- How does monitoring your blood pressure affect your motivation to care for your heart health? Filtered by age or net household income (n = 471)
- S. Cheng, V. Xanthakis, L. M. Sullivan et al. (2012), Hypertension, 60, 1393. https://doi.org/10.1161/HYPERTENSIONAHA.112.201780